This is the second article in a series of ‘Billing Issues’ that practices around the nation are facing.
The healthcare industry has gone through significant changes over the past decade, including an increase in deductibles, which has effected payment collections. In the midst of these changes, keeping a steady cash flow for a practitioner is like slaying a dragon.
When it comes to generating revenue, physicians cannot rely on insurance collections alone. Therefore, they will have to redesign their workflows to meet new challenges presented by payment collections, which are a major chunk of their overall income stream.
Following are five effective steps that can help you streamline, or re-design your workflow to improve patient collections:
- Create payment policy and share it with patients
What good is your self-payment policy if your patients are not informed about it? Develop a comprehensive self-pay policy centered on your specialty. Communicate your practice’s payment policy to your patients. Explain to the patients their financial obligations, and help them create a plan to pay their outstanding dues.
A comprehensive payment policy should:
- Communicate its clauses clearly to the patients
- Improve the relationship between patient and practice
- Ensure an organized collection process
- Avoid legal implications
While creating a policy for your practice, make sure of the following:
- Policy is written in simple language, so that patients can understand and follow it completely.
- Policy is comprehensive enough to include problems specific to the patients who visit your practice.
- Staff – medical and administrative – is on board with the policy. They have a comprehensive understanding of the policy, so that they can communicate and discuss it with patients. Similarly, if your practice has more than one physician, then educate them about the policy, and the impact of patient payments on the practice.
- Be mindful of the ethnic and cultural diversity among your patients, and translate the policy in all possible languages so that your patients understand it properly.
- Ask for, and use feedback from your patients to review and amend the policy, as needed.
- Ask the patients to sign the policy at the time of registration, so that it has legal standing in case of non-payment or delays from patients.
- Collection at the time of new appointment
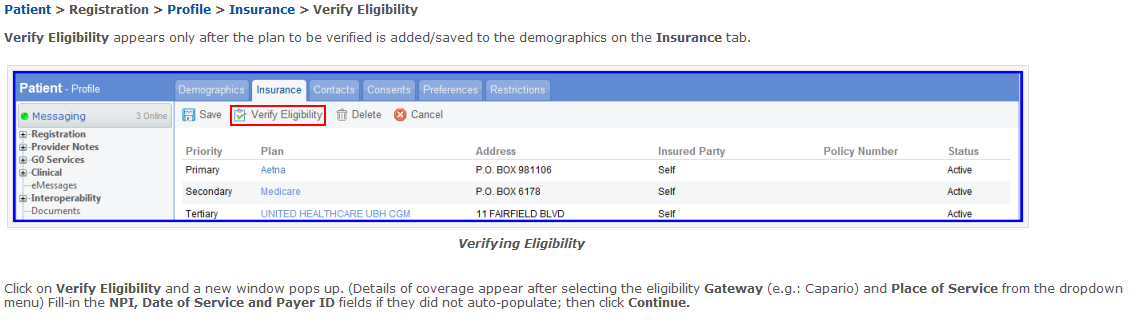
The time to determine the patients’ ability to make timely payments, is when they are scheduling an appointment. Take a holistic approach while taking down details of the patient – demographic and insurance – and verify insurance eligibility on the spot via Electronic Health Records (EHR). Make sure that you take down accurate details, because incorrect information will result in delayed payments.
- Opportunities to collect payments from check-in to check-out
Collecting deductibles and co-payments at the time of service should be a permanent part of the practice workflow. The best time to collect patient payments is during registration, and just before the patient is taken to the exam room. Once the front-desk staff loses this opportunity and the patient steps out of the practice, it becomes more difficult to collect payment.
How to ensure ‘at-time-of-service’ collections:
- Learn the art of asking patients for payments:Teach your staff to ask the right questions while dealing with patients at the front-desk. One question your staff should refrain from asking the patients is: “Would you like to pay now?” Instead train them in asking politely and professionally, “How would you like to make your payment?” This will give a clear message to the patient that the practice expects payment before service.
- Be flexible with the mode of payment:These days, most people refrain from carrying cash with them,so don’t hesitate to accept all forms of payments – cash, personal checks, debit or credit card. You can further facilitate patients and increase the possibility of payments, by setting up an ATM at your practice.
- Save credit card details for future billing:Some patients may hesitate, but most of them – usually the regular ones – will find it convenient to have their credit card details saved with the practice. An integrated solution of EHR and Practice Management System is beneficial in this regard, which will enable the administrative staff to keep a record of the patient credit card information and billing.
- Determine the amount of copays:The information collected at the time of appointment, can be verified with insurance payers, to help determine the copays to be collected. However, EHR can give you the patients’ insurance coverage with a single click. Once the front-desk has the information of the deductibles, and the covered medical services, they can ascertain the copay to be collected.
- Include past payments in the bill:While preparing the bill for patients, include outstanding balance, which will automatically populate in the e-Super bill. In case, patients fail to clear previous bills, hand them a copy of the printed statement at check-out.
- Coordinate with patients to make a payment plan:This applies to those patients who are negligent of their financial responsibilities, or are unable to make complete payments. At the time of check-out, have a meeting with them, and map out a way to collect maximum possible payments.
- On leaving the exam room:As the patient exits the exam room, the physician should remind them to consult the administrative staff at check-out before leaving. This is to impress upon the patient, the importance of paying their dues.
- Don’t delay the follow-up procedure
No matter how efficiently your staff follows at-time-of-service strategy, there are going to be unpaid claims and patient balance. However, try to make maximum collections during the first week of posting the first statement. The more you delay in following up the patient payment, higher the chances that it won’t be paid.
- Call the patient:Physicians consider it the most effective way of recovering debts. If your staff has accurate contact details, then there should be no delay in reminding patients of their unpaid medical bills. In order to make the call more effective, design a script to remind the patient in a polite, yet assertive manner. You can also send automated text message from your EHR to remind patients of their payments.
- Remind them through e-mail:Owing to the debt culture in our country, likelihood is that patients have prioritized their debt claims. Therefore, billing staff should set automatic e-mails to remind patients of their financial obligations to your practice.
- Utilize Patient Portal:Implementing an EHR system at your practice makes patient collections efficient and convenient for the patient and the practice. They can log on to patient portal, using the login detail provided by the staff, and make their payments. Practitioners can also save time and money, by sending patient statements via the patient portal.
- Test and review your workflow
This can also be called the ‘testing’ phase of the new workflow. Maintain a record of the revenue and patient payment collections during the testing phase, and compare with the previous record to see if the workflow has been successful.
In case of unsuccessful implementation:
- Go back to the first phase to measure staff readiness
- Get feedback from everyone involved in the change
- Find any setback in allocating financial resources
- Identify gaps in the workflow design, and its implementation
If your analysis reveals improvement in the process of patient collections, then make efforts to sustain the change.
- Get feedback from staff and patients
- Reward your staff to increase efficiency
- Include staff in your success story
- Document the journey for future change
What Next?
Watch our webinar on demand, “Patients Collections: 7 mistakes your practice should avoid” to understand and review your patient collection process. You can also call us to schedule a free consultation on medical billing 212-852-0279 (384).
