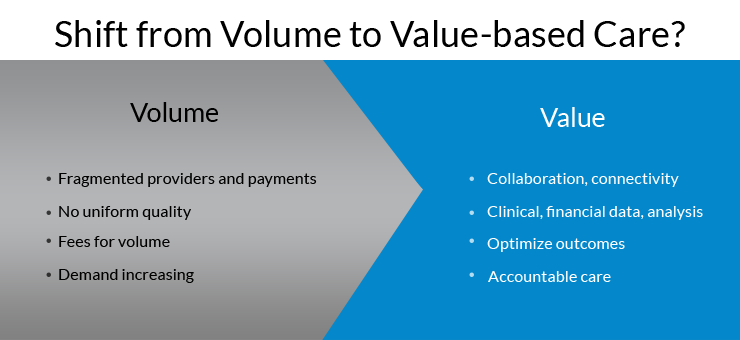
An expected shift is going to take place soon in the health industry, where healthcare will transform from volume based (paid for every patient visit) to value based (paid for quality of service). The government is encouraging physicians to form Accountable Care Organizations (ACOs), so that they can cut down on costs and provide quality patient care in limited resources, shared among them.
The evolution from fee-for-service to value-based service is quite challenging as it requires implementation of electronic systems, training staff, and smooth functioning of the changed workflow.
Introducing ACO
Centers for Medicare & Medicaid Services (CMS) described ACOs as “groups of doctors, hospitals, and other health care providers, who come together voluntarily to give coordinated high quality care to their Medicare patients.”
The purpose of this system is to ensure quality care to patients, particularly to those with chronic diseases to ensure that they get proper care at the right time. Often physicians fear to make the shift from volume to value based care because of money, time and adaptation of new workflows. However, the transition period can be made smooth by adopting the implementation tactics discussed below.
Fear of the change
According to a survey conducted by Purdue Healthcare Advisors from hospital administrations, 46% of respondents said that they had “no plans to implement an ACO in near future.” Among the “no plans” hospitals, 52% said the idea of ACO is too vague to be implemented and require more proof for its success. 49% of the “no plans” group said their practices were too small to make the change and 26% did not see any potential profits from this change. These reservations and fears, as shown by the survey are valid and make the move from volume-based to value-based medical services complicated.
Government incentives can help physicians to meet their financial loss and spearhead the transition process. However, these incentives take time coming through and may provide physicians a temporary cushion but are not the long term solution. Physicians must make changes to their own workflow in order to reap continuous benefits.
Preparing for the change
There are different ways through which physicians can cut cost and implement the volume to value service at the practice.
- Physicians can make use of the freestanding centers for testing, surgery and intensive care units instead of the hospital settings that can help to cut costs.
- Physicians can get registered with the insurances that provide incentives on utilizing generic medications. This initiative gives doctors huge sums of money in savings.
- Electronic Health Record (EHR) has the ability to monitor patients with severe medical problems and diseases. Physicians who have implemented this system at their practices would help physicians provide quality care through efficient data gathering, sharing and monitoring. For example, EHRs can help pediatricians by sending them alerts about children with overdue immunizations. Physicians can contact the parents and set an appoint to vaccinate kids on time. This way they can provide value-based service and avail incentives on time.
- Sharing resources among a group of physicians or co-management can help reduce costs and reap benefits. Physicians with small practices can come together to form an ACO and bring their resources – material, financial and human – together to cut down on extra costs. This way, physicians can provide value-based service in limited resources.
- In July 2013, Centers for Medicare and Medicaid Services (CMS) reported that ACOs that implemented the change during early years of the government announcement were able to reduce costs by 0.5 % when compared with the non-ACO practices. Therefore, it’s suggested to make the shift early to acquire more benefits.