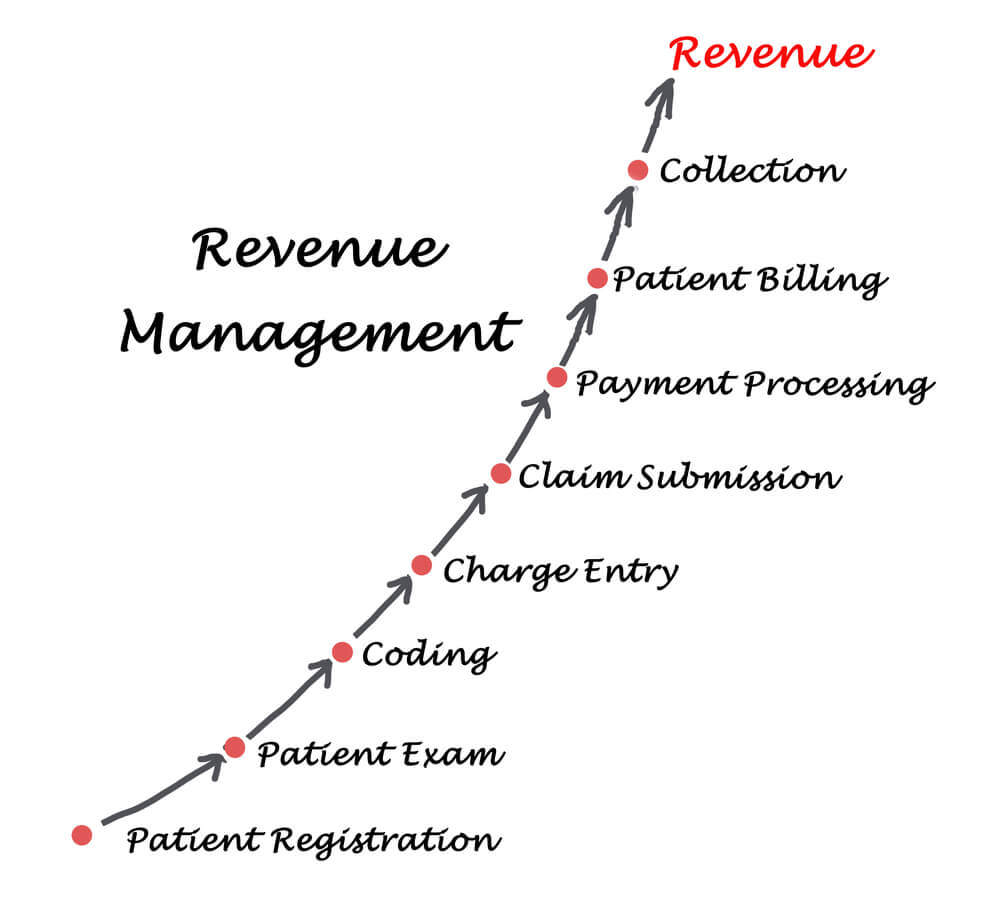
Revenue cycle management (RCM) is an important process for running a thriving practice. The financial, and ultimately administrative, the success of any practice is a function of how well designed and efficiently enacted its RCM system is. Fortifying the financial front is crucial for a number of obvious reasons, like designing and employing marketing strategies thereby attracting more patients, workplace and workforce expansion, etc. A reliable RCM also helps identify, track and mitigate any loopholes that might encumber and consequently derail the operational efficiency of the billing process at any level from the beginning, when claims are submitted, through end, when payments are completed. Addressing the indicated loopholes can substantially reduce and eliminate any potential delays and loss of revenue that the practice might experience otherwise.
Qualification and productivity of the staff involved, incorporation of strategies for smooth processing of claim submission, payment posting, reviewing error and denials, etc., and utilization of technology, are some key requisites needed for designing workflows that maintain a high degree of efficiency at every point.
Following are some strategies that, when incorporated intelligently into your existing RCM, can help improve its efficiency extensively:
Bringing an experienced billing service provider onboard

The most promising approach to regulate and improve your practice’s RCM is to outsource it to an experienced billing services provider; CureMD Medical Billing Service is an end-to-end revenue cycle management solution geared towards more than 32 specialties, with its staff actively overseeing and managing entire billing operations; from claim creation, quick submission, robust follow-up, denial management, appeals, payment posting, reporting as well as consistent training practice staff to get paid, on average, 6% more and 35% faster. It is an excellent option for practices seeking to augment their revenue management mechanism but lacks the adequate expertise required to execute the aforementioned wide range of tasks on their own.
Regular Claim Audits

Claim denials are an unavoidable part of the healthcare process. While practices won’t be able to eliminate them entirely, there are steps that can be taken to reduce their occurrence and to make sure they, or the reasons they originate from, are not repeated. Placing checkpoints at each stage of the cycle for regular audits will help identify the causes behind the denials, and to devise effective strategies for addressing the indicated causes.
Process in smaller batches

The volume of claims being processed at a given time also affects the efficiency of an RCM system. Larger volumes can result in a greater number of mistakes and errors thereby undermining the procedural reliability of the entire RCM process. Processing claims in smaller batches reduces the frequency of mistakes perpetrated thus allowing your staff to focus on each claim. individually. Or alternatively, entrust your RCM responsibilities to a billing service provider like CureMD capable of managing enormous volumes of billing processes swiftly and with outstanding adeptness.
Prepare and analyze reports

What better way to evaluate growth and/or shortcomings than to zoom out a bit from the quotidian to view the big picture i.e., through monthly, quarterly and yearly reports. Generating reports for a wide variety of financial metrics help practices monitor trends in their growth, the proportion of paid and denied claims, etc. These reports give a clear indication of the financial standing of the practice, while also showing a clearer picture of areas that need greater attention.